Brief Summary
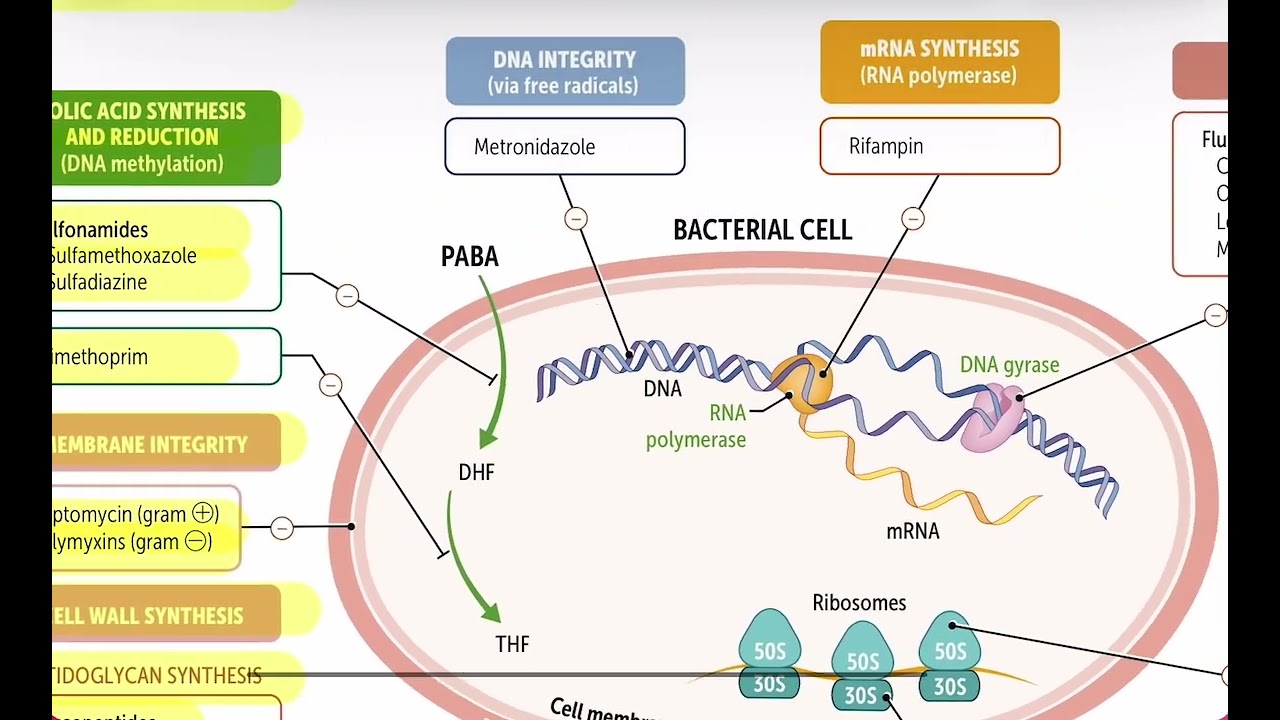
This video provides an overview of antimicrobial therapy, explaining how different antimicrobials target essential processes within bacterial cells. It covers mechanisms of action, clinical uses, and resistance mechanisms of various antibiotics, including penicillins, cephalosporins, carbapenems, and others. The video also discusses specific drugs and their effects on folic acid synthesis, cell wall synthesis, membrane integrity, DNA integrity, mRNA synthesis, and protein synthesis.
- Antimicrobial therapies target essential bacterial processes.
- Key targets include folic acid synthesis, cell wall synthesis, DNA/mRNA synthesis, and protein synthesis.
- Resistance to antimicrobials often involves enzymatic inactivation or mutations in target proteins.
Introduction to Antimicrobial Therapy
Antimicrobial therapy functions by targeting key processes within bacterial cells. These processes include folic acid synthesis and reduction, which are essential for DNA methylation. Sulfonamides, such as sulfisoxazole and sulfadiazine, act as structural analogues of PABA, blocking dihydropteroate synthase and preventing dihydrofolic acid synthesis. Trimethoprim inhibits dihydrofolate reductase, preventing the conversion of dihydrofolate (DHF) into tetrahydrofolate (THF).
Cell Wall Synthesis Inhibitors
Cell wall synthesis is another critical target for antimicrobials. Peptidoglycan synthesis is inhibited by glycopeptides like vancomycin and bacitracin. Peptidoglycan cross-linking is blocked by several classes of antibiotics, including penicillins and cephalosporins. Penicillin-sensitive penicillins include penicillin G, penicillin V, ampicillin, and amoxicillin. Penicillin-resistant penicillins include oxacillin, nafcillin, and dicloxacillin, while antipseudomonal penicillins include piperacillin.
Cephalosporins and Other Cell Wall Inhibitors
Cephalosporins are divided into five generations: first-generation (cefazolin, cephalexin), second-generation (cefuroxime, cefoxitin, cefaclor), third-generation (ceftriaxone, cefotaxime), fourth-generation (cefepime), and fifth-generation (ceftaroline). Carbapenems include imipenem, meropenem, and ertapenem. Monobactams include aztreonam.
Membrane and DNA Integrity
Membrane integrity can be disrupted by daptomycin, which acts on gram-positive bacteria, and polymyxins, which act on gram-negative bacteria. DNA integrity can be affected via free radicals by metronidazole. DNA gyrase, essential for DNA replication, is inhibited by fluoroquinolones such as ciprofloxacin, levofloxacin, and moxifloxacin.
mRNA and Protein Synthesis Inhibitors
mRNA synthesis, dependent on RNA polymerase, can be inhibited by rifampin. Protein synthesis is targeted at the bacterial ribosome. At the 50S subunit, chloramphenicol, clindamycin, and linezolid act. Macrolides such as azithromycin, clarithromycin, and erythromycin also act on the 50S subunit. Streptogramins like quinupristin and dalfopristin inhibit protein synthesis at this site as well. At the 30S subunit, aminoglycosides including gentamicin, neomycin, amikacin, tobramycin, and streptomycin block protein synthesis. Tetracyclines such as tetracycline, doxycycline, and minocycline, along with glycylcyclines like tigecycline, also inhibit the 30S ribosomal subunit.
Penicillins: Mechanism, Use, and Resistance
Penicillin G (available in intravenous and intramuscular forms) and penicillin V (available in oral form) are prototype beta-lactam antibiotics. They act as structural analogues of D-ala-D-ala, binding to penicillin-binding proteins (PBPs), also called transpeptidases. This blocks transpeptidase-mediated cross-linking of peptidoglycan in the bacterial cell wall and activates autolytic enzymes, further weakening the cell wall. Clinically, these drugs are primarily used against gram-positive organisms such as Streptococcus pneumoniae, Streptococcus pyogenes, and Actinomyces. They are also used against gram-negative cocci, mainly Neisseria meningitidis, and spirochetes, most importantly Treponema pallidum.
Penicillins: Spectrum, Adverse Effects, and Resistance
Penicillins are bactericidal for gram-positive cocci, gram-positive rods, gram-negative cocci, and spirochetes. However, they are beta-lactamase sensitive, meaning they can be inactivated by this enzyme. Adverse effects include hypersensitivity reactions, direct Coombs test-positive hemolytic anemia, and drug-induced interstitial nephritis. Resistance occurs through beta-lactamase, which cleaves the beta-lactam ring, or through mutations in penicillin-binding proteins.