Brief Summary
This video provides a comprehensive overview of urinary and bowel elimination, focusing on terminology, normal processes, common problems, and care guidelines. It covers topics such as urination, catheterization, bowel movements, enemas, and ostomies, offering practical advice for healthcare providers and caregivers.
- Key terms and definitions related to urinary and bowel elimination.
- Guidelines for normal urination and catheter care.
- Different types of catheters, enemas, and ostomies.
- Procedures for collecting urine specimens and assisting with elimination.
Introduction to Urinary and Bowel Elimination
The video introduces the topic of urinary and bowel elimination, emphasizing the importance of understanding key terms to fully grasp the subject matter. It sets the stage for a detailed discussion on the processes and potential issues related to these essential bodily functions.
Defining Key Terms Related to Urination
The lecture defines urination, micturition, and voiding as the process of emptying urine from the bladder. A normal person produces about 1500 ml of urine in 24 hours, while a patient with a urinary catheter should produce 30 ml per hour. Normal urine is yellow, clear, and without a distinct or foul odor. Any abnormalities, such as cloudiness or blood, should be reported immediately due to potential infection or bleeding.
Rules for Normal Urination
Several rules for normal urination are outlined, starting with practicing medical asepsis by wearing gloves to protect oneself and the patient, and following standard precautions for bloodborne pathogens. Providing adequate fluids is crucial for flushing out infections and hydrating the patient. Healthcare providers should follow the patient's voiding routines, assist them to the bathroom, and help them assume a normal position for voiding. Privacy should be provided, and running water or music can help mask voiding sounds. Perineal care is necessary for incontinent patients to prevent infection and skin problems.
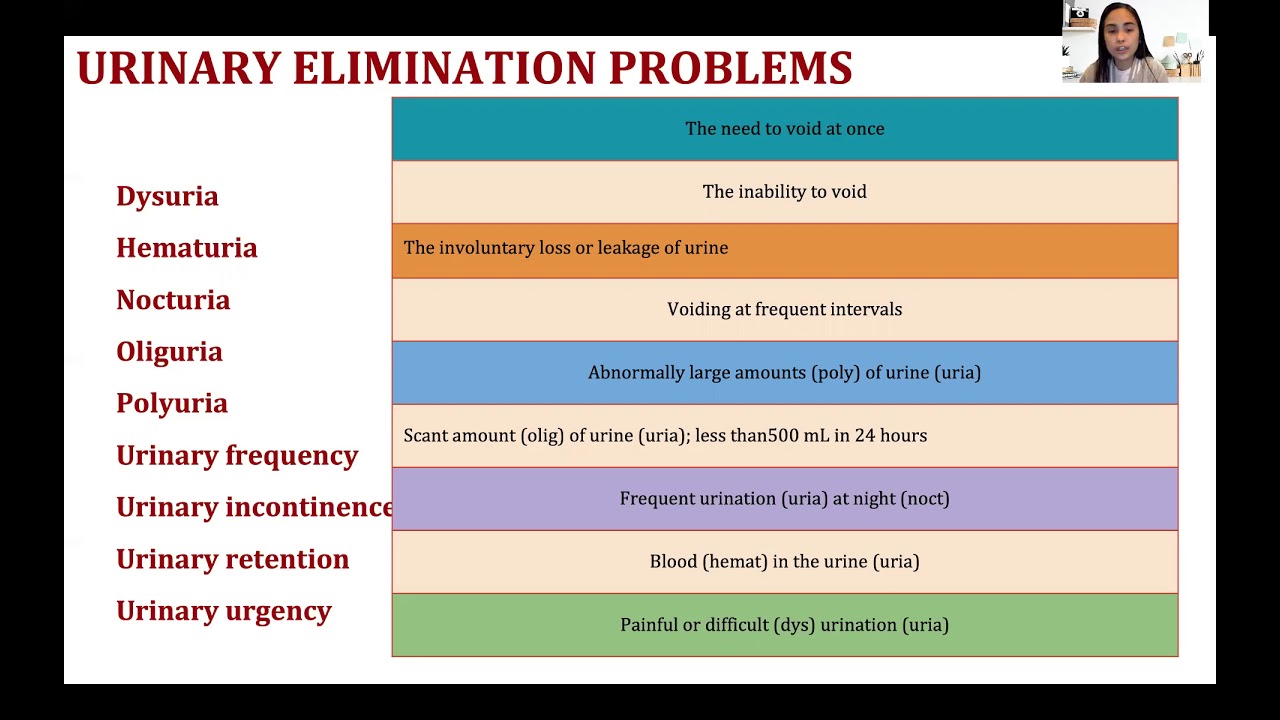
Matching Medical Terms to Definitions
The video reviews medical terms related to urinary issues, matching them with their definitions. Urinary urgency is defined as the need to void at once, while urinary retention is the inability to void. Urinary incontinence is the involuntary loss of urine, and urinary frequency is voiding at frequent intervals. Polyuria refers to abnormally large amounts of urine, oliguria is a scant amount of urine (less than 500 ml in 24 hours), and nocturia is frequent urination at night. Hematuria is blood in the urine, and dysuria is painful or difficult urination.
Understanding Catheters
Catheters are defined as tubes used to drain or inject fluid through a body opening, with catheterization being the process of inserting a catheter. Catheters are used to collect urine specimens, especially when a patient cannot pass urine or has urinary retention. It's important to collect specimens from the catheter itself, not the urinary bag.
Types of Catheters
The lecture describes different types of catheters. A straight catheter drains the bladder and is removed immediately, used temporarily for conditions like urinary retention after spinal anesthesia. An indwelling Foley catheter, also known as a retention catheter, remains in the bladder for an extended period to measure urine output and monitor urine consistency. A suprapubic catheter is an indwelling catheter inserted through a surgical incision in the suprapubic area. Lastly, a condom catheter is applied externally like a condom and connected to a drainage bag, mainly used for urinary incontinence, though it can be easily removed.
Guidelines for Handling Urinary Catheters
Guidelines for handling urinary catheters include following medical sepsis rules and standard precautions. Urine should flow freely without kinks in the tubing, and the catheter should remain connected to the drainage tubing. The drainage tube should be kept below the bladder to prevent backflow and infection. The drainage bag should be attached to the bed frame, not the side rails, and should not rest on the floor. The catheter should be secured to the inner thigh, and the care plan should be followed for catheter care, typically done daily or after bowel movements. The drainage bag should be emptied at the end of each shift, with the amount of urine measured and recorded.
Additional Catheter Care and Observations
Additional guidelines include encouraging fluid intake unless contraindicated, and promptly reporting any complaints of pain, burning, or irritation to the nurse. The color, clarity, and odor of the urine should be regularly checked, along with the presence of particles or blood. Signs and symptoms of urinary tract infections (UTIs), such as fever, chills, flank pain, changes in urine, and altered mental status, should be observed. Urine leakage around the catheter should also be monitored. The video mentions upcoming hands-on demonstrations for emptying urinary drainage bags, removing indwelling Foley catheters, applying condom catheters, and bladder training. Bladder training involves clamping the catheter tubing to encourage the patient to recognize the urge to void, helping them regain normal urinary function.
Introduction to Bowel Elimination
The video transitions to bowel elimination, defining peristalsis as the alternating contraction and relaxation of intestinal muscles that facilitate the movement of stool and nutrient absorption. Feces are the semi-solid waste products in the colon, while stool refers to the excreted feces. Defecation is the process of bowel movement.
Factors Affecting Bowel Elimination
Several factors affecting bowel elimination are discussed, including privacy, habits, diet, fluid intake, activity level, drugs, disability, and aging. Privacy is essential, as some individuals cannot defecate if observed. Habits, such as a regular morning routine, should be respected. A diet lacking in fluids and fiber can lead to difficulties in bowel elimination. Physical activity promotes bowel regularity, while certain drugs can affect stool consistency or cause diarrhea. Disabilities and aging can also impact bowel elimination, with older adults often experiencing decreased peristalsis and constipation.
Defining Bowel Elimination Problems
The lecture defines common bowel elimination problems. Fecal impaction is the prolonged retention and buildup of feces in the rectum. Diarrhea is the frequent passage of liquid stools. Fecal incontinence is the inability to control the passage of feces and gas. Constipation is the passage of hard, dry stools, and flatulence is the excessive formation of gas in the stomach and intestines.
Bowel Training and Enemas
Bowel training aims to help individuals gain control of bowel movements and develop a regular elimination pattern, often involving exercises. Enemas involve introducing fluid into the rectum and lower colon to remove feces, relieve constipation or fecal impaction, and clean the bowel before surgeries or diagnostic procedures. The patient should be positioned on their left side for effective administration.
Types of Enemas
Different types of enemas are described, including tap water enemas, saline enemas (a solution of salt and water), soap suds enemas (using castile soap), and small volume enemas (commercially prepared solutions). Oil retention enemas use mineral, olive, or cottonseed oil. Hypertonic solutions pull fluid out of interstitial spaces but are contraindicated for dehydrated patients and young infants.
Rectal Suppositories
Rectal suppositories, cone-shaped solid drugs inserted into the rectum, are discussed as a method to aid bowel movements. They are used for constipation, fecal impaction, and bowel training. The suppository should be moistened with water or lubricating jelly before insertion, and the patient should lie on their left side with the right knee bent.
Understanding Ostomies
Ostomies are surgically created openings for the elimination of body waste, often necessary when the rectum cannot function properly due to conditions like terminal cancer. A stoma is the opening seen through the abdominal wall. Colostomies are created in the colon, while ileostomies are created in the ileum (small intestine).
Nursing Care for Ostomies
Nursing care for ostomies includes changing the pouch every three to seven days to prevent infection and draining the bag when it is one-third full to prevent it from bursting. Patients should be instructed to decrease intake of gas-forming foods like cabbage and potatoes to prevent flatulence. The stoma should be cleaned with warm water, avoiding disinfectants that can cause irritation.
Assisting with Elimination and Elimination Equipment
Assisting with elimination involves using various equipment such as bedpans, urinals, and commode chairs. A commode chair is a chair frame with a toilet seat and removable collection bucket for weak or unsteady individuals. Bedpans are used for both urination and defecation, while urinals are specifically for male patients to urinate.
Guidelines for Assisting with Elimination
Guidelines for assisting with elimination include honoring the person's requests, providing privacy, ensuring the call light and toilet paper are within easy reach, and providing good perineal care. Hand washing should be encouraged for infection control. Gloves and appropriate PPE should be worn. Waste should be observed for any unusual characteristics like blood or cloudiness. Bedpans and urinals should be removed promptly and never placed on the over-bed table. Air fresheners should be used to address odors, and equipment should be disinfected according to hospital policy.
Collecting Urine Specimens and Urinalysis
Different methods of collecting urine specimens are outlined, including routine urine specimens, clean-catch specimens (collecting urine mid-stream), and 24-hour urine collections (used to check for kidney stones). A 24-hour collection involves discarding the first urine and collecting all subsequent urine for 24 hours, keeping the collection container on ice. Urinalysis, the examination of urine under a microscope and by chemical means, is a commonly used diagnostic tool.